TREATING LOW BACK PAIN WITH LUMBAR STEROID EPIDURAL INJECTIONS
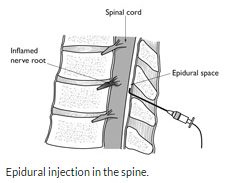
Epidural steroid injections deliver medication directly (or very near) the source of pain generation. In contrast, oral steroids and painkillers have a dispersed, less-focused impact and may have unacceptable side effects. An epidural steroid injection delivers steroids directly into the epidural space in the spine. Sometimes additional fluid (local anesthetic and/or a normal saline solution) is used to help ‘flush out’ inflammatory mediators from around the area that may be a source of pain.
Epidural injections are often used to treat radicular pain, also called sciatica, which is pain that radiates from the site of a pinched nerve in the low back to the area of the body aligned with that nerve, such as the back of the leg or into the foot. Inflammatory chemicals (e.g. substance P, PLA2, arachidonic acid, TNF-α, IL-1, and prostaglandin E2) and immunologic mediators can generate pain and are associated with common back problems such as lumbar disc herniation or facet joint arthritis. These conditions, as well as many others, provoke inflammation that in turn can cause significant nerve root irritation and swelling.
The epidural space encircles the dural sac and is filled with fat and small blood vessels. The dural sac surrounds the spinal cord, nerve roots, and cerebrospinal fluid (the fluid that the nerve roots are bathed in).
Typically, a solution containing cortisone (steroid) with local anesthetic (lidocaine or bupivacaine), and/or saline is used.
Steroids inhibit the inflammatory response caused by chemical and mechanical sources of pain. Steroids also work by reducing the activity of the immune system to react to inflammation associated with nerve or tissue damage. A typical immune response is the body generating white blood cells and chemicals to protect it against infection and foreign substances such as bacteria and viruses. Inhibiting the immune response with an epidural steroid injection can reduce the pain associated with inflammation.
Several common conditions that cause radiculopathy – severe acute or chronic low back pain and/or leg pain – (sciatica) that can be treated with steroid injections include:
A lumbar disc herniation, where the nucleus of the disc pushes through the outer ring (the annulus) and into the spinal canal where it pressures the spinal cord and nerves.
Degenerative disc disease, where the collapse of the disc space may impinge on nerves in the lower back.
Lumbar spinal stenosis, a narrowing of the spinal canal that literally chokes off nerves and the spinal cord, causing significant pain.
You will lie face down on a table or special bed. The doctor might give you a sedating medication. The epidural injection takes place in several steps:
•The skin will be cleaned and injected with an anesthetic to numb it.
•The doctor will insert a needle through the skin toward the spine.
•The doctor will use a machine that produces live X-ray video called fluoroscopy. With it, the doctor will maneuver the needle between the bones of the spine.
•Using a contrast dye, the doctor will confirm the needle is placed in the epidural space. That’s the space between the spine and the spinal cord inside it.
•When the needle is in position, the doctor will inject a solution into the epidural space. The solution contains a steroid medicine, also called corticosteroid, and usually an anesthetic medicine, too.
•The epidural injection is usually not painful because of the numbing medicine used at the start. Many people do have mild tenderness for up to a few days after the injection.
Although many studies document the short-term benefits of epidural steroid injections, the data on long-term effectiveness are less available. Indeed, the effectiveness of lumbar epidural steroid injections continues to be a topic of debate. This is accentuated by the lack of properly performed studies.
For example, many studies do not include use of fluoroscopy or X-ray to verify proper placement of the medication despite the fact that fluoroscopic guidance is routinely used today. Additionally, many studies do not classify patients according to diagnosis and tend to ‘lump’ different types sources of pain together. These methodological flaws tend to make interpretation and application of study results difficult to impossible.
The patients that we’ve treated at Michigan Sports and Spine Center have reported significant pain relief after the injections. The reason for that is injections are only part of the treatment plan. We continue care after the injections with medications, physical therapy, and home exercise programs that help patients get back to the life they love.
ABOUT MICHIGAN SPORTS & SPINE CENTER:
We’re innovative leaders utilizing cutting-edge technologies such as musculoskeletal ultrasounds, PRP, stem cell treatment, and other innovative procedures. Michigan Sports & Spine Center is committed to resolving your pain, not simply masking it. We treat the whole body, not just the injury, and perform preventative treatment so your injury doesn’t come back. Our studies prove that Michigan Sports & Spine Center has patient success rates much higher than the national average. We treat everyone from high-profile athletes to your neighbor next door. Our primary focus is getting our patients back into the game of life!
